1. Continuous Monitoring
Use Case: Monitoring cardiovascular conditions of a heart disease patient
Wearable sensors are the patches of an electrocardiogram that continuously measure patients heart rate, rhythm, and electrical activities. Devices give real-time updates in cardiovascular conditions for the patient, which is then transmitted to healthcare providers who can identify abnormalities such as arrhythmias or signs of heart failure early on to act accordingly.
Example: For patients who have suffered heart attacks, there is a smart ECG patch. It will detect abnormal heart rhythms when such a patient goes about carrying out his or her routine activities and alert the cardiologist in charge of the patient. The provider will then view the recorded data, immediately call the patient and inform him or her of the incident, advise on hospitalization and thus prevent a probable cardiac event.
Use Case: Continuous Glucose Monitoring (CGM) for Diabetes
Patients with diabetes are benefited by continuous glucose monitoring. It is small sensors implanted into the body that sense glucose levels of people at all times throughout the day and report their findings directly to the patient and copies for the treating physicians in real-time to help them in the management of blood glucose levels and the doses of insulin.
Example: A juvenile diabetic patient wears a CGM device that can send alerts to the patient and his caregiver whenever glucose levels are above or below the threshold, especially at night. The caregiver receives alerts directly on the phone so that insulin or sugar is administered timely to prevent a dangerous episode of hypoglycemic events.
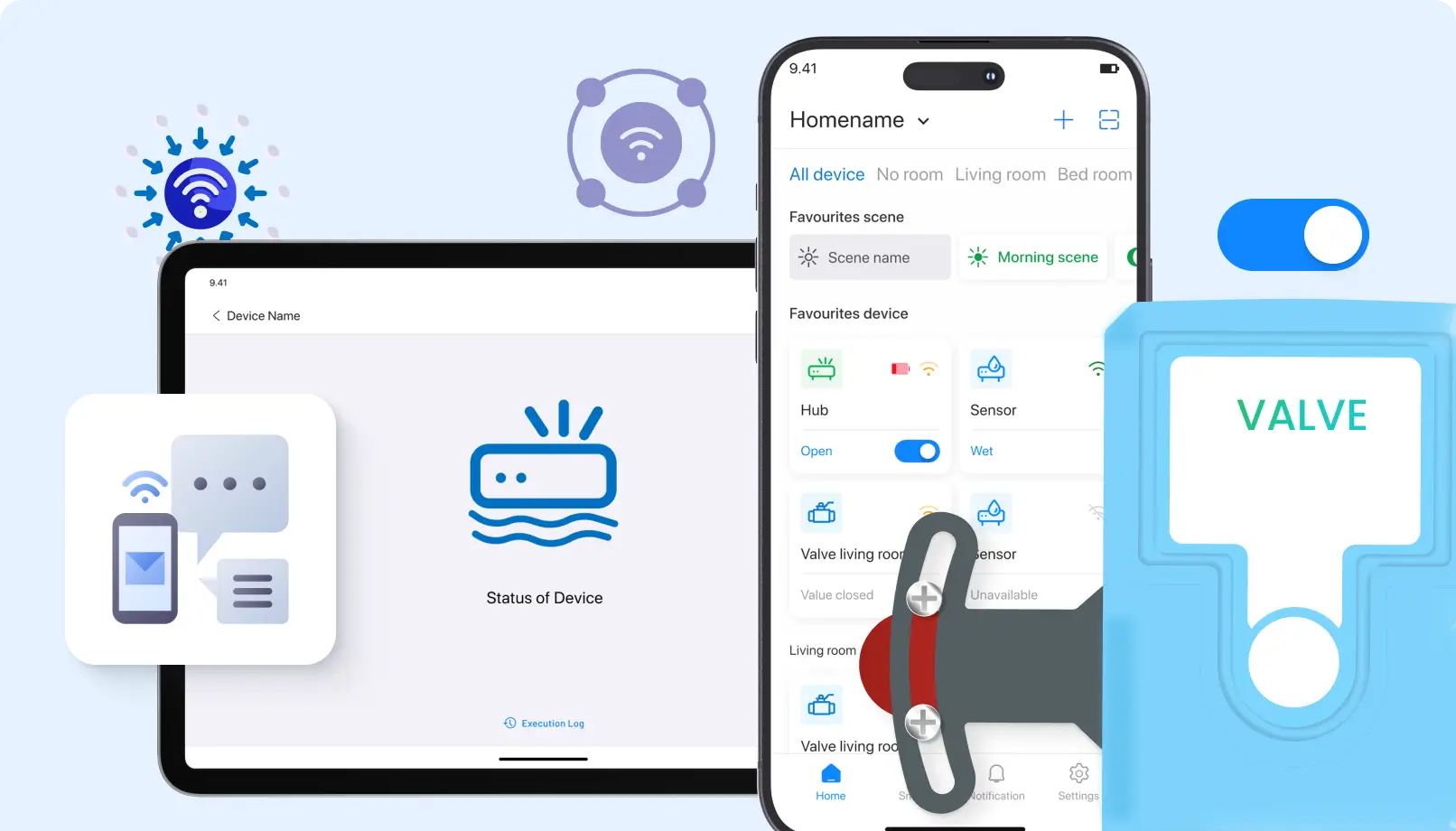
2. Remote Patient Monitoring (RPM)
Use case: Remote monitoring of patients post-surgery
Patients often are monitored for their healing after surgery to avoid complications like infections and blood clots. The remote monitoring systems comprise various sensors that measure other very important vital signs such as temperature, heart rate, and oxygen level. Remote monitoring systems allow doctors to take care of patients even from their home and decrease the chances of readmission in hospitals.
Example : A patient who has just gone under major abdominal surgery is moved out of the recovery room with a smart wearable device attached to his body. The device captures body temperature and blood pressure readings and transmits them to the RPM system of the hospital. Providers there review the data and note that the patient’s fever is rising; this is one of the earliest signs of developing infection. The patient is instructed to visit an ER immediately and receive treatment before the infection gets worse.
Use Case: RPM for Geriatric Patients with Chronic Disorders
In turn, the elderly patients suffering from chronic conditions, for example, COPD or heart failure, are tracked at their homes by a group of sensor devices tracking respiration, heart rate, and the level of physical activity. The information garnered in such a method can be transmitted to the caregivers and health care professionals who are well-equipped to respond immediately to a deteriorating condition.
Example: A 75-year-old patient suffering from COPD is given a wearable sensor to measure her oxygen saturation and respiration rate. At one point in the evening, the sensor captures a considerable decrease in oxygen saturation and therefore irregular breathing. An alert is sent to the patient’s medical provider automatically, who then calls the patient for check-up and arranges for oxygen aid to be administered at home.
3. Early Disease Detection
Use Case: Cancer Biomarkers Detection
Biosensors were designed to detect specific biomarkers that indicate the existence of cancer, present in fluids like blood or urine. The key feature of such sensors is early detection of diseases such as prostate or breast cancer before a clinical sign or symptom appears, meaning intervention can be carried out much sooner than it would be possible otherwise, along with better opportunities for treatment.
For instance, PSA levels in blood are detected by biosensors to monitor regularly for men at risk for prostate cancer. The sensor relates elevated PSA levels to further diagnostic testing that diagnoses the case as early-stage prostate cancer, and hence its patient seeks early treatment and, therefore, drastically improves the prognosis.
Use Case: Wearable Sensors for Neurodegenerative Diseases
Wearable sensors track changes in motor function as well as neurological signals to be able to monitor for diseases such as Parkinson’s or Alzheimer’s. The anomalies in gait and movement and cognitive patterns tracked by these sensors are very useful in making an early diagnosis.
Example: An elderly patient’s gait and balance are monitored by an intelligent insole embedded with sensors. The stream from the sensor indicates early signs of abnormalities in their gait, which normally are symptomatic of Parkinson’s disease. The neurologist gets back to the patient, and further tests confirm it to be Parkinson’s disease, thereby allowing an early intervention to delay its progression.
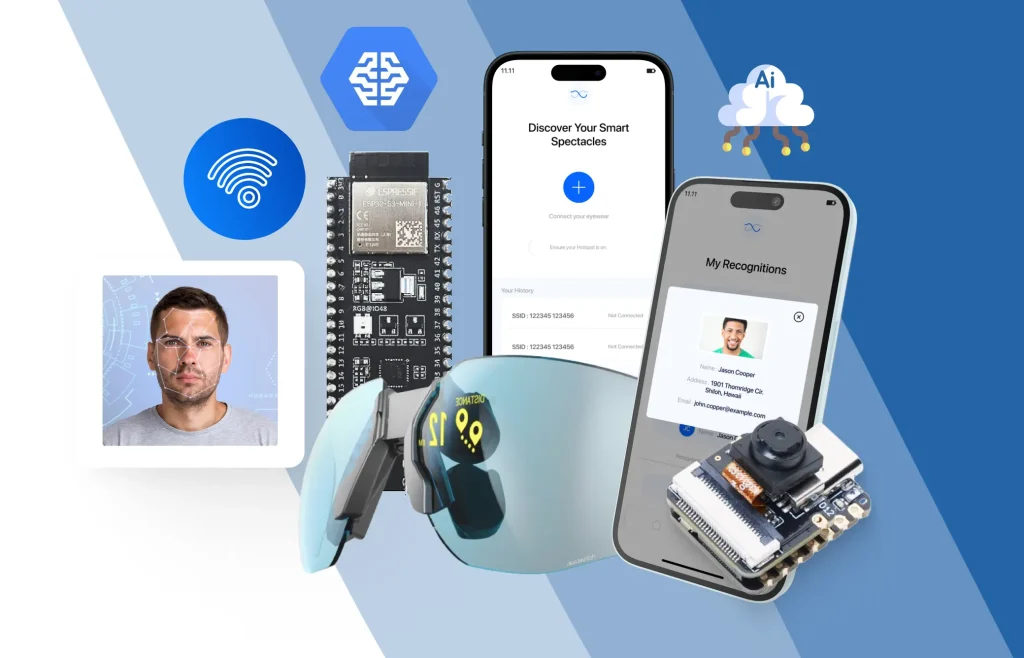
4. Smart Wearables and Implants
Use Case: Smartwatches on Cardiac Health
Modern smartwatches come equipped with sensors that monitor heart rate, oxygen saturation levels, and execute on-demand ECG. These patient-owned monitors enable a patient to take an active role in monitoring his health with the same information sent back to their healthcare providers through connected health platforms.
Example: A 60-year-old patient wears a smart watch that monitors heart rate variability and performs ECG. One evening, the watch does detect atrial fibrillation (AFib), and it immediately notifies both the patient and his doctor. He goes to the hospital, and further testing confirms AFib, so he can be treated promptly with anticoagulants before it can become an AFib-related stroke.
Use Case: Implanted Sensors for Chronic Pain Management
Implanted biosensors may measure electrical nerve and muscle activity to provide data about chronic pain states. Such devices connect to outpatient equipment that allows patients to modify their pain management therapies, for instance electrical nerve stimulation, in real time.
Example: A patient with chronic back pain has an implanted sensor monitoring nerve activity and signals transmitted to a wearable device to deliver spinal cord stimulation. The device automatically adjusts its stimulation based on real-time data on levels of pain that the sensor has detected, so as to yield the most relief without medication.
5. Medication Management
Use Case: Smart Pill Boxes for Medication Adherence
Medication adherence is a key component of chronic illness management, yet patients often forget to take their medications. Smart pillboxes-the sensitizing-enabled product-track whether a patient has taken his or her prescribed medication and sends reminders if a patient misses a dose to the patient or alerts to a caregiver.
Example: An elderly hypertensive patient takes blood pressure drugs daily using a smart pillbox that tracks the daily intake. One day the system senses a missed dose and sends a reminder via a mobile app. As time goes on and the dose is not administered, the system alerts the daughter of the patient so that timely action is taken.
Use Case: Injectable Sensor-Based Drug Delivery Systems
The injectable sensors could measure the amount of drugs flowing in the blood so that the patients are given the correct dosage. They are very helpful for patients subjected to chemotherapy as well as hormone administration, where correct levels of medication have to be maintained at specified levels in the blood.
Example: A cancer patient who receives chemotherapy uses an injectable sensor that takes real-time measurements of drug levels every now and then. The sensor detects that the drugs in the current dose cannot reach an optimal level, so the doctors adjust the dose to ensure appropriate treatment of the patient.
6. Emergency Response
Use Case: Fall Detection in Elderly Patients
Falling is a significant issue among elderly patients living independently. It can monitor the sudden movements of an elderly person or the lack of movement after falling and send alerts to the emergency services or caregivers.
Example: The elderly patient, who experiences falls in the past, is equipped with a smart device that is recording her movement and body balance. She had one accidental sudden fall in the afternoon; soon, the sensor sent an alert automatically to her caregiver and nearby emergency medical team. The paramedics have reached immediately so that the major complications due to fall could be avoided.
Use Case: Heart Attack Detection
Real-time monitoring of the activity going in the heart through sensors can quickly find abnormal ECG readings, indicative of the very first symptoms of a heart attack, and alert the healthcare providers to begin immediate action.
Example: A middle-aged patient with a history of cardiovascular disease wears a chest patch which continuously monitors heart function. The sensor identifies abnormal heart activity that indicates that a heart attack has begun. A warning is issued to the patient’s cardiologist and the local emergency services. The patient is rushed into hospital where proper treatment is administered before the damage has a chance to occur.
Conclusion
Sensor technology in healthcare has, instead of just keeping patients under watch, provided real-time information that has facilitated early detection of disease through clinicians and timely management of chronic conditions while responding swiftly in emergencies. The use cases enable appreciation of the breadth of benefits sensor technology will be used to provide personal, continuous, efficient care toward improved patient outcomes as well as quality of life. Through smart wearables, implants, and remote monitoring systems, the healthcare sector is turning more proactive, data-driven, and accessible while bringing the future of care into the present.